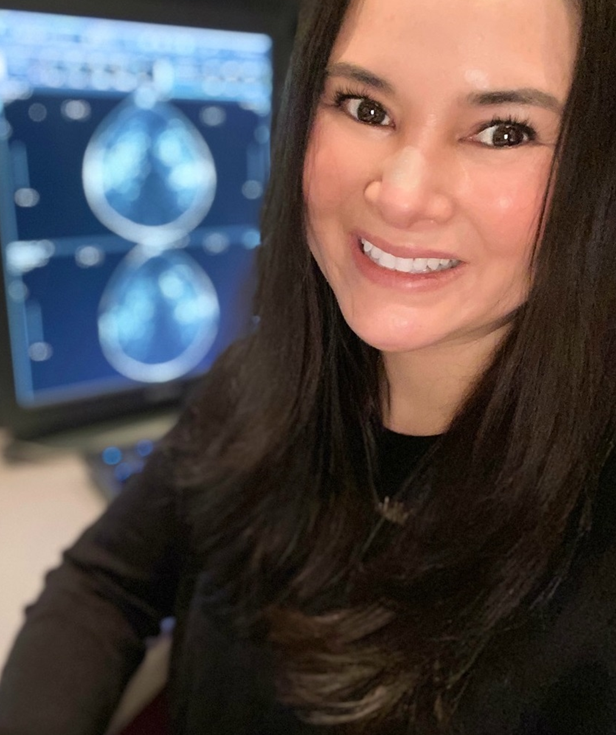
Dr. Taylor Loon MBBChBAO, PGY-1 Diagnostic Radiology, SUNY Upstate Medical University
Dr. Taylor Loon MBBChBAO, PGY-1 Diagnostic Radiology, SUNY Upstate Medical University
I was once in a patient handoff where the resident doctor had a transgender male patient on their service. While discussing the patients care with myself, they frequently stated the patients deadname (calling a transgender person by their birthname when they have changed their name as part of their gender transition)1 and commonly referred to the patient as “she” rather than “he”. After multiple attempts to correct this resident’s comments, I felt unsuccessful in trying to change their outlook towards transgender patients in their care. Being a member of the LGBTQ+ community myself, I began to wonder despite commitments to patient care equity, how do we be better regarding care of our transgender and non-binary patients?
Barriers to Access of Care
Lesbian, gay, bisexual, transgender and queer or questioning + (LGBTQ+) experience higher rates of healthcare disparities compared to their heterosexual or cisgender counterparts. Identifying factors contributing to these disparities have included perceived discrimination from health care providers and denial of healthcare, in addition to racial identity and geographic location2. Published in 2020, the Trans PULSE Canada project collected survey data from 2873 trans and non-binary people in Canada in 2019. 45% of the participants reported having 1 or more unmet healthcare needs in the year 2019.2 This is compared to 4% of the general Canadian population in the year 2015.2 In addition, 12% of patients avoided going to the emergency department altogether due to their trans identity, despite needing care. Past history of harassment, or fear of harassment was reported to be a major contributor to resistance to healthcare access by those patients in the study. 2
How Can We Improve?
A mini-guide into common definitions
It is without a doubt that we as medical professionals want to provide the highest quality care to our patients in an open and judgmental-free way. However, for many this may be challenging due to lack of familiarity of understanding the correct terminology regarding the patient’s gender identities. The list below is a mini-guide into common terminology.
Transgender or trans: “an umbrella term for people whose gender identity (a person’s internal, deeply held sense of their gender, their ‘maleness’ or ‘femaleness’) and/or gender expression (the external presentation of gender, such as name, clothing, hair, voice, and/or body characteristics) differs from what is typically associated with the sex they were assigned at birth”2
A transgender patients identity does not depend on physical appearance, if they are taking hormonal therapy, or if they undergone any surgical procedures (gender confirmation surgeries). In addition, make no assumption based on their appearance alone and believe patients when they tell you that they are trans.
Non-binary, gender non-conforming or genderqueer/genderfluid: “terms used by people who experience their gender identity and/or gender expression as falling outside or somewhere in between what is typically associated with being a ‘man’ or ‘woman’”2
These definitions are much different than transgender and should not be used interchangeably. They should only be used if the patient self-identifies as non-binary or gender non-conforming
Two Spirit: “Two-spirit” refers to a person who identifies as having both a masculine and a feminine spirit, and is used by some Indigenous people to describe their sexual, gender and/or spiritual identity. As an umbrella term it may encompass same-sex attraction and a wide variety of gender variance, including people who might be described in Western culture as gay, lesbian, bisexual, transsexual, transgender, gender queer or who have multiple gender identities.”3
Cisgender: a term for people whose gender identity matches the sex that they were assigned at birth. 2
Using Preferred Terminology
Very commonly, the name and pronoun of the patient you are caring for may not be what they choose to identify with. Changing names and genders on medical records may often be extremely challenging for patients and thus resulting in the information not being up to date. Calling a patient by the wrong name or “deadnaming” a patient can put them in an incredibly uncomfortable position.
When first meeting a patient, ask them how they would like to be addressed and, if they are comfortable sharing, what pronouns they use. In addition to making sure other staff members in the department use the preferred pronouns and names of patients, check that medical documentation includes this information as well. If unable to change the patient’s name in a medical record, put their preferred name in parentheses beside and only use their preferred and pronouns name when dictating, writing progress notes or procedure notes.
Creating a Welcoming and Supportive Environment
So how exactly can interventional radiologists achieve this? One simple way to make your department or practice more inclusive is the use of signs, stickers, and flags such as the LGBTQ+ pride flag and the transgender and nonbinary flags. It is a small, simple gesture that can help create ease in patients and let them know that your practice is a safe space where they are able to seek care.
Another way to support patients is to avoid unnecessary gendering in forms, procedures, and medical documentation. A first step would be to avoid using gendering language such as “sir”, “maam”, or “miss” when addressing patients. Providing gender neutral bathrooms and change rooms, having a patient write their gender identity (if needed) on any medical forms rather than a tick box of male vs female, providing patient gowns that are comfortable and covering a range of individuals are a few small steps to decrease unnecessary gendering.
Most importantly, make sure yourself, colleagues and staff are trained in these practices. Every provider in your department from radiologists to nurses to techs should be educated in how to make sure trans, two-spirit and non-binary patients are treated with respect and dignity every step in their care. Colleagues should be corrected if still using incorrect terminology in regards to a patient’s identity. Organizations such as Rainbow Health Ontario and Trans Care BC offer on-demand and scheduled courses for healthcare providers to increase both clinical and cultural competency in treating LGBTQ+ patients and creating an inclusive environment.
Inclusivity is not about creating unnecessary changes and policies to a department or practice nor is it an overnight process. By understanding the needs of our trans and non-binary patients, we can help create a strong patient-provider relationship and provide safe and welcoming interventional radiology departments.
References
1Stowell, J. T., Grimstad, F. W., Kirkpatrick, D. L., Brown, L. R., & Flores, E. J. (2019). Serving the Needs of Transgender and Gender-Diverse Persons in Radiology. Journal of the American College of Radiology, 16(4), 533–535. https://doi.org/https://doi.org/10.1016/j.jacr.2018.12.050
2Trans Pulse Canada. (2020, March 10). Health and health care access for trans and non-binary people in Canada. Retrieved October 26, 2021, from https://transpulsecanada.ca/results/report-1/.
3Fewster, P. H. (n.d.). Two-spirit community. Researching for LGBTQ Health. Retrieved October 27, 2021, from https://lgbtqhealth.ca/community/two-spirit.php.