Access Menu
CAIR WIR Spotlight - Dr. Ethel Rivas Zuleta
CAIR WIR Spotlight - Dr. Rebecca Spouge
CAIR WIR Spotlight - Dr. Elizabeth Dave
CAIR WIR Spotlight - Dr. Aida Ahrari
CAIR WIR Spotlight - Dr. Fiona Anyumba
CAIR WIR Spotlight - Dr. Alda Tam
Call for CAIR Award 2024 Nominations
Combined Interventional/Body Radiologist – Hamilton General Site, ON

Dr. Virani grew up in the Greater Toronto Area and pursued undergraduate and graduate studies at Western University. He returned to Toronto for medical school before venturing out east for Diagnostic Radiology residency at Dalhousie University in Halifax. Dr. Virani has spent the last two years at Emory University in Atlanta, Georgia completing IR training. He looks forward to returning home to Canada to spend time with family while enjoying some travelling. Dr. Virani will be starting locums around the country and his goal is to join a radiology practice with an IR group possessing an innovative spirit, looking to push the boundaries to improve patient care.
Why did you choose the USA for fellowship?
I always wished to experience some level of training in the United States, to see how things were like south of the border. I had opportunities to pursue this for medical school and residency, however for different reasons at the time, I chose to stay in Canada, and had wonderful training experiences in Toronto and Halifax. Therefore, I saw fellowship as my last chance to pursue training in the US.
What was the interview and decision process like?
Unlike Canada, fellowship training programs in the US still may participate in a match process for candidate selection. For radiology, IR, Neuro, MSK, and Breast fellowships participate in a match conducted by the National Residency Match Program. So, just when I thought I was finished with the high-anxiety provoking morning of “clicking a mouse button to determine my future”, I was not.
Similar to the Canadian Resident Matching Service process, I was required to submit the usual gauntlet of documents such as essays, CV, and reference letters to the central match database. Since I knew I wanted to at least keep the option of fellowship training in the US a possibility, I had completed the United States Medical Licensing Examinations (Steps 1 to 3) during my medical school and PGY-1 years. To this day I am not sure if Emory IR required these exams or not, but I knew I did not want these to be a defining obstacle to a great training experience.
I applied to at least 10 different IR programs across the US, coast to coast. I knew IR fellowship programs were competitive the year I applied but I did not realize just how competitive. I was granted an interview at only one US institution – Emory University in Atlanta, Georgia.
I flew down for my scheduled interview not knowing what to expect. Immediately, I was blown away by the university and hospital campus infrastructure. My interview day consisted of meeting other candidates socially followed by a brief group meeting with the new program director – Dr. Bill Majdalany, who moved from the University of Michigan to Emory to begin as the program director. I then proceeded to complete four 1-on-1 interviews throughout the day with Emory IR faculty. Before I knew it, my interview day was complete and I was on a flight back to Halifax.
A few weeks later, while in Washington D.C. for the well-known AIRP (American Institute for Radiological Pathology) course, I received an email from Dr. Majdalany inquiring if I was attending the SIR (Society of Interventional Radiology) annual conference, which was only a few weeks away. I was not planning on attending SIR since I was already at AIRP and had several resident clinical duties waiting for me back at Dalhousie. However, I knew it may be in my best interest to have more face time with the Emory group, not to mention the director of the training program. I decided to fly to Austin, Texas to spend 2 days at the SIR conference, during which I had breakfast with Dr. Majdalany (possibly the most important breakfast in my life to date). I’ll leave the details of our conversation out, but needless to say during my flight back home I knew Emory was my destiny.
Several months later during the summer of 2019 I once again had to make that mouseclick – and of course the rest was history.
Why Emory?
Where do I begin? I think Emory is unique in being one of the few institutions across the country offering a near complete IR fellowship training experience. Being the largest hospital system within the state of Georgia, the majority of complex cases are filtered to Emory, and the catchment does not stop at the state border, as we treat patients from Florida, South Carolina, Alabama, and beyond, including far internationally. The strength of the IR fellowship begins with the department, which houses the largest number of IR faculty in the country, including several past SIR presidents, with training backgrounds literally coast to coast who are eager to teach. Emory is a leading transplant and oncology center, not to mention supports one of the busiest trauma hospitals in the nation. We also rotate through the Children’s Healthcare of Atlanta hospitals, having the privilege to learn innovative interventional radiology techniques and skills in a quaternary pediatric setting. However, I feel most importantly, Emory from day one of the fellowship, stresses the importance of clinical training in shaping a successful interventional radiologist. In the ever-changing field of IR, Emory emphasizes the consulting nature of the IR specialty, and teaches the fellow responsibility in managing the patient before, during, and after a procedure.
What was an average day as a fellow like?
My alarm would ring at 4:30 am. I would arrive at the hospital by 6:00 am. Depending on the hospital site I was rotating through, I may or may not be with additional fellows (a total of 7 of us spread across 5 hospital sites). We would round on the in-patient list and write daily progress notes. The day’s scheduled inpatient/outpatient list of procedures were worked up either the night prior or early in the morning. We would tend to any overnight pressing matters. Morning rounds begin between 7:00 to 7:30 am depending on the hospital site. During this time, the IR trainee discusses each case for the day with the attendings, detailing the procedural plan. Upon the completion of rounds, we would be ready for the day’s cases to commence, typically the first case starting at 8:00 am. The main Emory University Hospital (where a fellow would spend 6 months of the year) typically has 4 angio suites available (and an additional CT room for cross-sectional procedures). An IR trainee is allocated to each room and is responsible for such during the day. At the additional sites, where only a single senior IR trainee is scheduled, we would be responsible for the entire day of cases. Once the last case has been completed, the fellow dictates the day’s cases while managing any floor issues that accrued. At this time, next-day planning occurs, consisting of triaging and working up inpatient consults to be scheduled around tomorrow’s outpatient list. It would not be unusual at the beginning of the year for me to walk out of the hospital after 9:00 pm, as I wanted the next day to run smoother than the last. Thankfully, as the training program progressed, I became more efficient at my duties, allowing myself to end the day earlier, slightly.
Overnight/weekend call coverage definitely had the potential to be busy. Due to the numerous sites covered by Emory we split the city into North and South calls, with a senior trainee and attending assigned to each daily. As Chief Fellow during my second year, I was responsible for the call schedule, ensuring trainees did not exceed a 1 in 4 call burden. The South pool was definitely on average the busier of the two pools, covering both Grady (level 1 trauma) and Emory University Hospital (transplant and complex surgical and hepatobiliary center). It was not uncommon to be up most of the night performing trauma embolizations or treating emergent bleeding patients, however we had an accepting culture of appropriate trainee reprieve following demanding shifts.
What was your case load?
After two years I would have completed slightly under 3000 cases with graduated autonomy. There is such a wide variety of cases performed at Emory, including great variation in complexity. My more complex case involvement included Transjugular Intrahepatic Portosystemic Shunt creation (commonly utilizing intracardiac echocardiography guidance for portal vein access), complex hepatobiliary interventions such as percutaneous transhepatic cholangiography with palliative stenting, cholangioscopy with lithotripsy and stone retrieval, complex organ and soft tissue thermal and chemical ablations, traumatic solid organ and pelvic embolizations, high volume liver-directed endovascular therapy including Y-90 radioembolizations, diagnostic and therapeutic lymphangiograms with embolizations, and complex venous reconstructions using intravascular ultrasound.
Emory’s strength in fellowship experience is the innovation in treating patients with complex diseases. For example, I have been involved in Emory’s early experience in endovascular arteriovenous fistula creation in patients requiring dialysis (we are now approaching 10 patients with endovascularly created fistulas). Additionally, Emory’s presence in pain and palliation has been second to none. In the hopes of curtailing the opioid epidemic, a consistent proportion of the training experience has been centered on pain interventions, including kyphoplasty (with thermal ablation of bone metastases), cryoneurolysis (with targets such as celiac plexus and pudendal nerves), and genicular nerve ablations for patients unable to undergo knee arthroplasty.
In what area, if anything, do you feel you were taught less?
I feel Emory has provided me with a very comprehensive fellowship experience, as highlighted above. However, following the trends across many American IR training centers, we are exposed to minimal aortoiliac and peripheral arterial disease cases, which is contrary to the Canadian fellowship experience to my knowledge. This disparity in training becomes revealed when searching for IR faculty positions in Canada. However, I would add that my imaging expertise and endovascular skills will allow me to get up to speed with these interventions. Emory has trained many fellows who have gone on to thrive in peripheral arterial disease practices. “Give a man a fishing pole” analogy comes to mind here.
What do you perceive as advantages and disadvantages of doing fellowship in the USA?
Before discussing the advantages and disadvantages between the two training environments, I feel a few things must be discussed. The first disparity coming to mind is the length of IR training between the US and Canada today. Due to the emergence of the IR residency training program in the US, there are now several routes to IR training. For example, a graduate from medical school can now be matched into an IR-Integrated residency program (internship + 5 years of IR training). The first 4 years are identical to Diagnostic Radiology (DR) training—and the trainee can sit for the diagnostic radiology boards. The final 2 years in this pathway are very IR heavy, including some non-IR training, commonly in the intensive care unit or in the surgical transplant service.
A second IR training route is to begin as a DR resident, then match into an Early Specialization in Interventional Radiology (ESIR) program. Here, the PGY-5 year of the DR program with the ESIR designation includes 7 months of IR including a month of non-IR. These trainees can then match into the second year of a 2-year Independent IR residency. The final year is completely dedicated to IR. Both routes are 6-year training programs.
Now, the conventional route of completing a 5-year Diagnostic Radiology residency followed by an IR residency is still a possibility, however the dedicated IR component is 2 years (total of 7 years of post-graduate training). I must also mention, there is NO MORE “IR fellowship” in the US. The three IR streams are all referred to as residency training programs.
The year I began my IR training in 2020 was the inaugural year of the two-year independent residency class. Initially when I was applying and became aware of this, I was quite deterred by the required extra year of training compared to Canadian IR fellowships. However, today, I would have it no other way. It took me a few months to even feel acclimated to Emory’s numerous hospital sites – let alone to a very different healthcare climate overall. Most importantly, the extra year of case experience in a trainee role was truly invaluable. I was able to hone skills in both common (such as uterine fibroid embolizations) and more uncommon procedures (such as prostate artery embolization or even percutaneous transesophageal gastrostomy tube placement). Therefore, all things considered, the extra year was definitely a bonus.
Secondarily, the 2-year IR residency program (not fellowship!) is advantageous for both academic and community career paths. For an academic path, the reasoning is fairly simple – two years of high-level clinical IR training in a very academic atmosphere sets the groundwork for academic IR success. However, I will also argue this pathway more so strengthens a candidate for community IR – where there may be a paucity of subspecialty services in one’s community hospital, where then the IR doctor can use their arsenal of knowledge and skills to improve patient care in multidisciplinary healthcare.
The disadvantages of an IR residency in the US are few in my opinion. The most difficult aspect was not seeing my family nearly as much as I wished during my training. Since the entirety of the fellowship occurred in the presence of COVID-19, especially the first year when case numbers were rising, it was not feasible nor practical to travel back home to Canada. Luckily, I was blessed with great co-fellows and attendings who made Emory feel like home.
I believe that secondary disadvantages, such as the lack of aortic and peripheral arterial disease training mentioned above, or even other procedural skills and knowledge that is emphasized in one country, or even institution, can be overcome with focused extra-training and mentoring. Basic guidewire and catheter skills along with diagnostic imaging expertise allows an IR doctor to succeed in unchartered territory. Mentors at Emory have emphasized to me not to overly-focus on a specific procedure, but to spend more time in understanding the disease process instead. The disease itself is far more likely to be around tomorrow compared to the treatment being offered today.
Are you planning on writing the Canadian VIR boards? Why or why not?
Yes, I am definitely planning on writing the Canadian IR boards. Similar to the American subspecialty IR examination, a standardized assessment of IR in Canada helps ensure those who practice within this field meet a standard competency of safety to best serve the patient.
Dr. Virani grew up in the Greater Toronto Area and pursued undergraduate and graduate studies at Western University. He returned to Toronto for medical school before venturing out east for Diagnostic Radiology residency at Dalhousie University in Halifax.
Dr. Supersad is currently a PGY-4 resident in diagnostic radiology at the University of Alberta. She was born and raised in Edmonton, and after medical school at the University of Calgary is back in her hometown to complete residency.
After growing up and completing medical as well as radiology training in Cape Town, South Africa (population approximately 5 million), Dr. Stefan Przybojewski, felt it was getting a bit small and was looking for adventure.
Through education, mentorship, and conversation this five-year program is on course to empower existing and future Women in Interventional Radiology.
Dr. Gilles Soulez MD, MSc, FSIR is a vascular and interventional radiologist at CHUM, University of Montréal. He completed his radiology residency in France at University Paris V in 1988 and completed a 2-year fellowship combined with a certification of the French College of Interventional Radiology.
Dr. Lindsay Machan is an interventional radiologist at the Vancouver Hospital, a CIRSE Distinguished Fellow, SIR Fellow and an Asia Pacific Society of Interventional Radiology Honorary Member
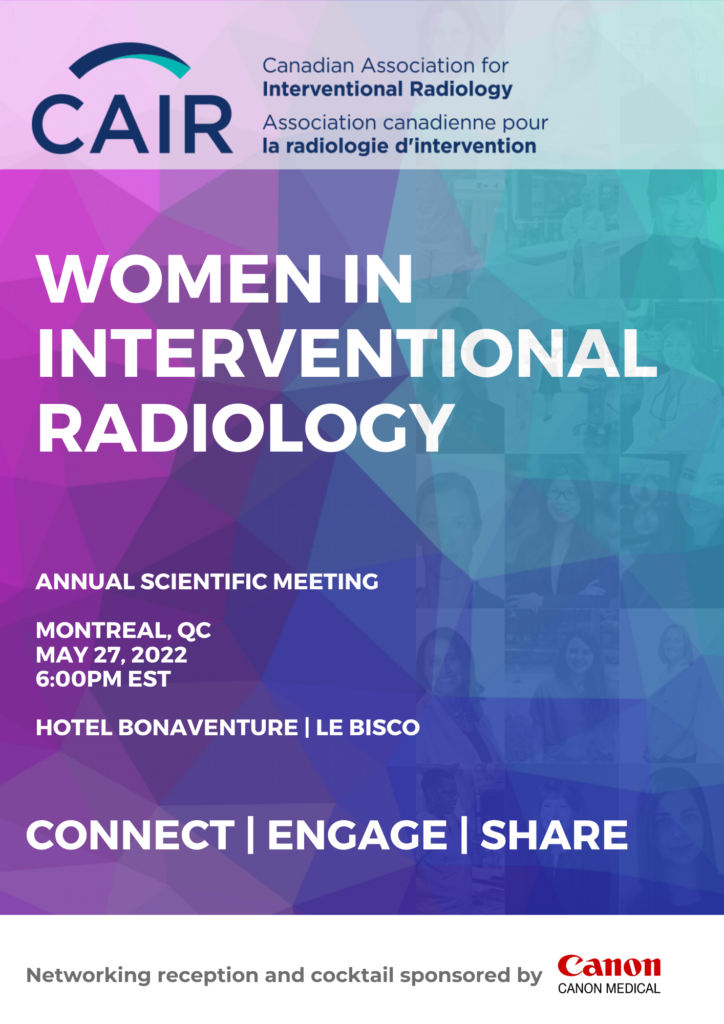
The Canadian Association for Interventional Radiology (CAIR) will be holding an in-person Annual General Meeting (AGM) for its voting members in good standing on May 27th, 2021 at 15:30 pm EST at Hotel Bonaventure in Montreal, during CAIR's Annual Scientific Meeting.
Dalhousie University Department of Radiology and Nova Scotia Health’s QEII Health Sciences Center Department of Diagnostic Imaging is offering a full-time faculty position for an Interventional Radiologist.
Dr. King is currently the lead for the Department of Interventional Radiology at the Peterborough Regional Health Centre.