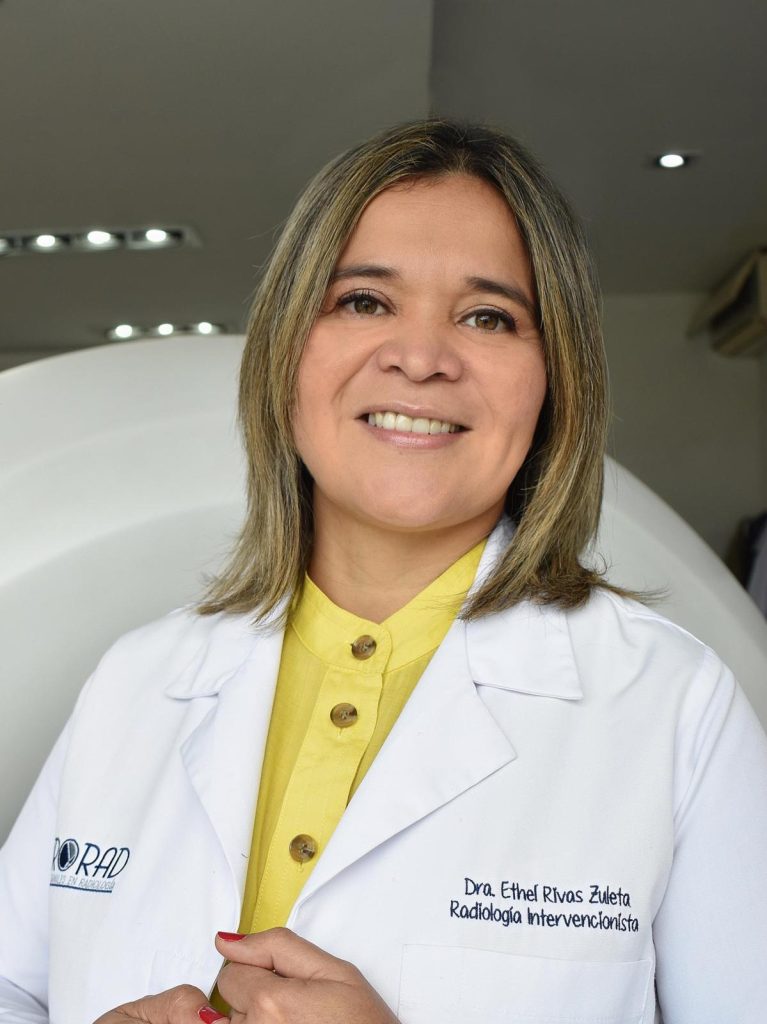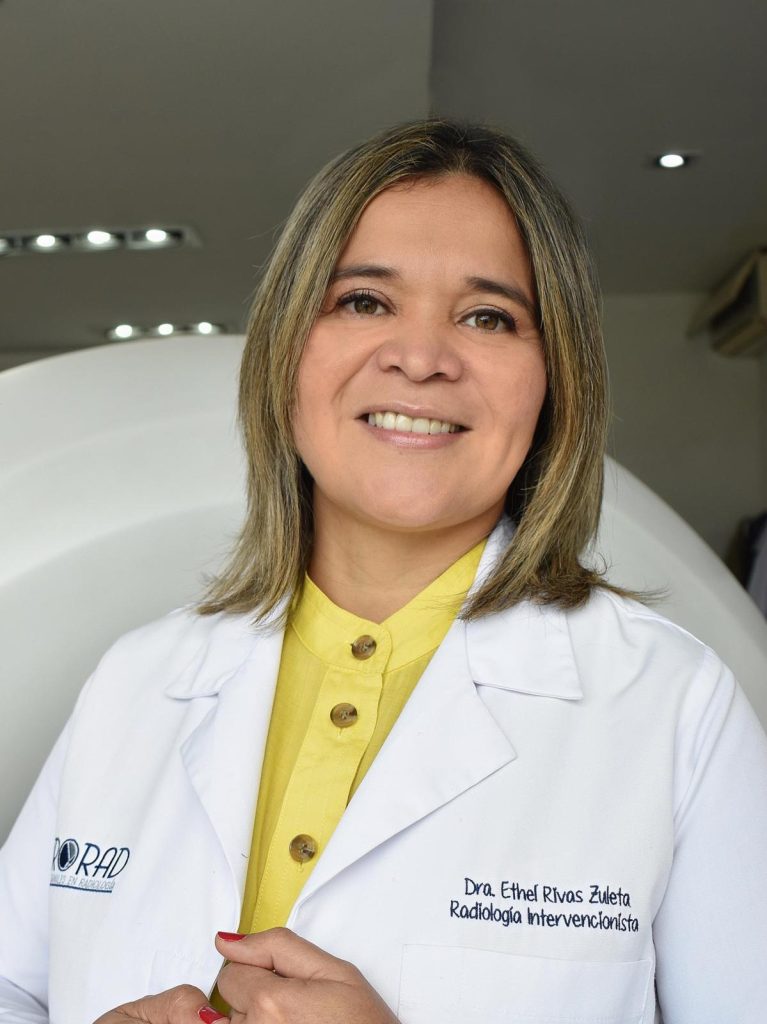
Can you share your journey into interventional radiology and what inspired you to pursue this specialty?
In my country (El Salvador); there was no one with the specialty of Interventional Radiology; so being a surgical resident, I was frustrated that many of the procedures had solutions that we only read about in books or magazines, which led me to the curiosity of said specialty, so after surgery I completed my residency in radiology with the purpose of finishing it and starting Interventional Radiology.
So during my residency in Diagnostic Radiology, I was curious to focus on Interventional Radiology, I tried to read about the procedures, and when I finished it, I looked in Latin America for countries where I could do it, which led me to visit different programs. It was in Mexico where I had the opportunity to do my fellowship.
How do you balance work and personal life in a demanding field like interventional radiology?
It is quite difficult in any specialty, especially those that involve shifts and procedures; however, I believe that being surrounded by people who not only understand you but also support you in all aspects of life is very important; and not only having the support of your partner but also of your children, parents, etc.
I have always thought that the correct balance is the one that gives you peace and makes you feel good because when you try to follow the standards of being an excellent mother, wife, daughter, friend, and colleague you end up on a path of burnout.
I have always thought that the correct balance is the one that gives you peace and makes you feel good because when you try to follow the standards of being an excellent mother, wife, daughter, friend, and colleague you end up on a path.
What are some key challenges you faced as a woman in interventional radiology, and how did you overcome them?
Being the first in my specialty, I not only faced some gender elements, but in general, in the entire surgical field of procedures, women often have to demonstrate that we are capable of performing them, in places where they are not accustomed to having a female voice leader. From nursing technicians, radiology technicians to the different medical specialties.
I was used to the operating room and dealing with many difficulties as a woman, but dealing with it as a team, then training all the staff, looking for the initial elements, and making sure they were available was more difficult since everyone expected me to demonstrate my skills, with my first procedures being “supervised” by surgeons or cardiologists to endorse my capability.
How has the landscape of interventional radiology evolved over the years, especially in terms of gender representation?
I am going to talk about my country and Latin America in general. Little by little, more women are involved in Interventional Radiology, as in the rest of the world. In countries like Mexico, Colombia, Chile, Brazil, and Peru, we already find women in leadership positions. This has opened more opportunities for women who want to dedicate themselves to the specialty.
In my country, we are already training three female interventionists and that would make us four.
What advice do you have for women who are aspiring to enter the field of interventional radiology?
It is a very complete specialty, in which you have the ability to intervene in many areas of medicine, and the important thing is to have a passion in everything you do, since from the smallest to the most complex procedure you are able not only to save lives but to carry out precise diagnoses and treatments with minimally invasive procedures.
To women: We are capable of developing ourselves in any area we get involved in, and the important thing is to believe in yourself, and to have the confidence that what you do will always be the best for you.
Are there any specific skills or areas of knowledge that you recommend focusing on during training for a career in interventional radiology?
I think that all areas are important, however it is important to take into account where you will be and where you will develop your work in the future; since many of us were trained in other countries and when we return to our countries of origin we get frustrated for not having everything that we have been taught; however, we can strengthen ourselves in areas such as oncology, pain, biliary, etc.
For people who train in a country with many opportunities, as with everything in medicine, it is always a good idea to rotate through all the areas and evaluate which one is of interest to you and try to strengthen that area.
Can you share any insights into the networking opportunities available for women in interventional?
Among the opportunities for exchanging ideas and knowledge are the Interventional Radiology meetings where you find forums and have the opportunity to meet leaders firsthand,
Also social media and open forums where you can interact and look for opportunities.
What role do you think diversity plays in enhancing the practice of interventional radiology?
We are a world with different opinions, people, races, genders; and that makes us what we are “human beings”; with incredible and different capacities that when together have always achieved the best.
Medicine in general should take advantage of the diversity of people, with different perspectives, realities, and experiences because we all have a common goal which is a “patient”; and that patient will also be full of diversity for which the contribution of everyone is important.
How do you see the future of interventional radiology, and what opportunities do you anticipate for women in the field?
Our specialty is growing every day, not only in numbers but also in areas such as oncology, vascular, pain, etc. In the future, I see a greater number of subspecialties within our field.
As for women, I am pleased to see women in leadership positions and, above all, maintaining that position.
Are there any specific organizations or conferences that you recommend for networking and career development in interventional radiology?
I think the Canadian Association for Interventional Radiology (CAIR) has done an excellent job, with areas focused on female leadership, opening up many opportunities.
I couldn’t mention a particular conference without underestimating the many that there are; the important thing is to be present and not be afraid to ask to participate and then you can see how the slightest contact or comment can lead to good results.
When I started Interventional Radiology I didn’t have the slightest idea who to talk to or where to start I went to a congress of my society (Ibero-American Society of Intervention) in Cancun, Mexico and I remember arriving at the registration table and finding a man in front of me and I asked him: Excuse me, Doctor, do you know who can help me train in Interventional Radiology? And coincidentally he was one of the founders of Interventional Radiology in Mexico, who was kind enough to take me to all the department heads of the area and I began to have contact with all of them.
What advice do you have for women in interventional radiology who are navigating leadership roles within the specialty?
The most important thing about leadership is to maintain it and take it over the long term, because we have very good leaders, however, maintaining that leadership is costly since it depends on many social factors.
It is always advisable when having a leadership position, to look for space and identify other women leaders who can accompany us in these tasks.
What aspects of the field/ your work do you dislike? How do you work around this?
I think that in my job what I don’t like are the changes in hospital policies or the lack of supplies that we sometimes face in underdeveloped countries because it leads us to levels of frustration that if we don’t know how to manage, lead us to levels of stress that are not healthy.
Have you encountered any specific stereotypes or misconceptions about women in interventional radiology, and how do you address them?
In general, women are always given special attention when it comes to handling stressful situations; since we are preconceived as emotional beings; therefore, we are often frowned upon even though our behavior is not different from that of our male colleagues. This leads many of us to want to develop masculine attitudes in order to be accepted, however, this is a mistake; since we must have counseling from both men and women for handling situations that bring emotions or work stress.
How do you handle situations where you may be the only woman in a professional setting, and what advice do you have for navigating such scenarios?
Always believe in yourself and your abilities. I believe that men and women have different behaviors and reactions, however, the certainty of believing in yourself and the confidence you have in yourself will be enough. Never try to act differently to impress. Everyone will be respected for their individuality.
What steps can women take to foster a supportive and collaborative community within the interventional radiology field?
Always identify a leader, whether male or female, who supports equality initiatives; as well as encourages activities among colleagues, and supports teams with nurses and technicians to maintain a team environment.
Problems between hierarchies between physicians and support staff are very common, however, having a collaborative environment makes work more comfortable and respectful.
Can you share any experiences or insights related to the integration of artificial intelligence in interventional radiology practice?
At the moment we have not had any integration with AI, however I know it will be very promising.
How do you balance the demands of interventional radiology with family responsibilities, and what advice do you have for women aiming to achieve this balance?
As doctors and people of science we are focused on achieving a 50/50 balance; however, in scenarios of procedures, emergencies, and night shifts, trying to achieve that balance is often impossible and leads to frustration and anxiety.
As I said previously, the important thing is to understand yourself, know your limits, and have a circle of trust in your partner or family, who understand your goals and support you.
Always knowing that you cannot be in everything at the same time will save you stress.
One must take advantage of the time you are free with the family to the maximum, disconnect a little,e and dedicate that quality time.
We must stop feeling guilty for not being able to be with the family all the time or try to be like other mothers or daughters, but rather feel satisfied with what we do. In your day-to-day life, work absorbs you, however, you can have quality time with your family with the same passion as you work.
Can you speak to any initiatives or projects you’ve been involved in that aim to address gender disparities or enhance the representation of women in interventional radiology?
At the last congress of my society, for the first time, there was a segment dedicated to women in Interventional Radiology; however, it was more of an empowerment approach; represented by a medical student, foreign doctors, and leaders in intervention, where our message to the entire audience was that we feel equally capable and now we need leaders who integrate us and give us opportunities.
I believe that women’s initiatives should be directed at promoting the leadership and guidance capabilities that we women have.
From this congress onwards, women’s leadership groups and the creation of support networks in the different Latin American countries will always be promoted.